Holy shit, y’all, I don’t even know where to start.
ETA: OMG. Love Tank just texted me to tell me that I accidentally wrote "2023" instead of "2024" in this blog post. I'm letting it stand as proof that THIS YEAR HAS KICKED MY ASS (and perhaps quite a few of my brain cells). You can make the appropriate date edits in your mind . . . unless yours is functioning like mine is.
2023 has been . . . A LOT.
Let me rephrase that: 2023 has been a Grand-Canyon-sized, festering cesspool of bloody, butthole-burning diarrhea.
With maggots.
And chitlins.
As I suppose is evident in the fact that it’s taken me until almost the end of April to tell y’all about it.
The nutshell is this: 2023 started—and remained—so full of craptasm that I vowed to start the whole year over on February 29.
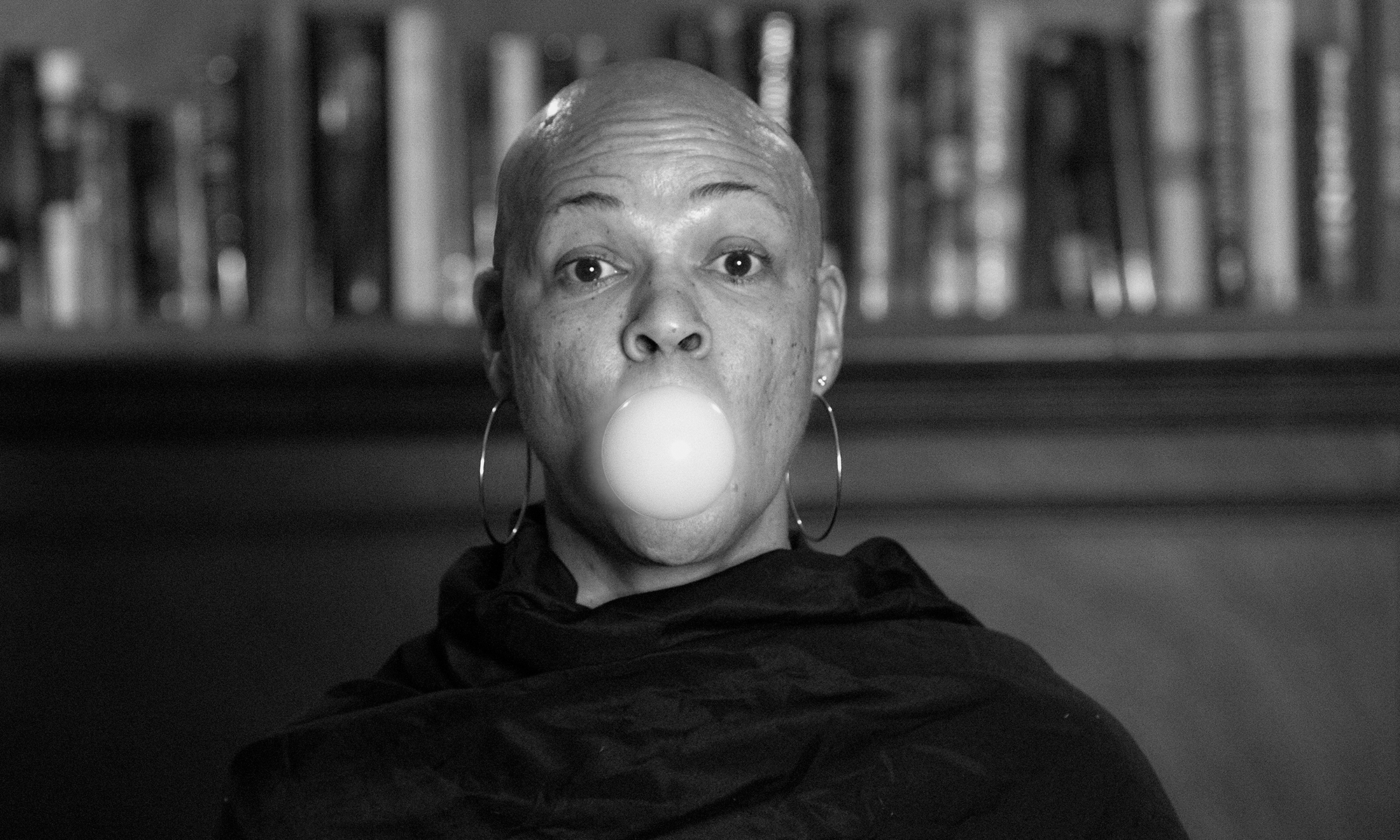
And although it’s lightened up a little, it hasn’t become the mountain of fuzziness and bliss I was hoping for. Yet here I am, feeling stronger and free-er of fucks, and I suppose that’s something to celebrate.
Because this blog is largely (supposed to be) about my cancer diagnosis, I’ll start by saying that I’m fine; I feel good, I have almost enough hair for the kind of half-ass ponytail you see on small toddlers, and the only medication that enters my bloodstream is Tylenol on occasion. As a bonus, I’ve dropped nearly 15 pounds with absolutely zero effort, thanks to the fact that nobody’s pumping me full of steroids. (This has motivated me to put in some effort to start getting back into shape—but so far, that effort has only extended as far as buying myself new HOKAs. But I digress.)
Aside from that, however, things pretty much started descending into the toilet the second week of January.
Buckle up, y’all. This is going to be a long one.
The ER from hell
Having spent nearly a month recovering from the December 12 reconstruction of my boobs, I was all set to return to work on January 10. The previous week, I’d been stricken ALL the way down with a dreadful bug which, despite the intensity with which it kicked my ass, refused to be identified as either the ‘Rona or the flu (I was 547% sure it had to be one of the two, because surely a mere cold wouldn’t be trying to kill me like this shit was . . . yet as miserable as I was in the week following celebration of the new year, COVID tests turned up nothing, and multiple thermometers returned only double-digit results).
Finally, on Sunday night, January 7, my mom called to check on me . . . and when I told her it seemed like I might live after all, she asked if I felt well enough to take her to the emergency room the next day.
When I tell you that set off ALL my alarm bells, I mean all the cathedrals, boxing rings, and middle school bell choirs in the world couldn’t compare to the jangling that suddenly arose from the depths of my psyche.
This is a woman who, several years ago, HAD A STROKE in the middle of hosting her bridge club—but because duty (in the form of coffee, dessert, and a few more bids) called, she kept right on keepin’ on, one hand curled in upon itself and useless, until the party ended—at which point, she allowed one of the ladies to drive her to Urgent Care. (Now. In her defense, she didn’t learn until much later that it had likely been a stroke; she was sent away from the Urgent Care facility with a shrug, as the hand had returned to normal by the time she was examined, and it wasn’t until a year or so later that she mentioned it to her doctor, who identified it as a small stroke. But still. HER HAND STOPPED WORKING and she kept right on refilling water glasses, y’all.)
This is a woman who, a couple of years ago, passed clean out in the middle of making breakfast in her apartment for me and my children; she paused mid-scramble and walked from her stove over to her sofa, complaining of fatigue and saying she needed to sit down for a second—and the next thing we knew, she was out like a light and unresponsive. She came to as I was rushing over to shake her, and insisted she was fine and did not need to see a doctor. A couple of minutes later, I looked over and she was drenched with sweat, soaking the front of her housedress. At that point, I INSISTED on taking her to the ER, and STILL she argued, until I threatened to knock her unconscious AGAIN and drag her there by her feet if she didn’t cooperate. She finally agreed, and spent a night in the hospital for observation, but ultimately the doctors blamed all the drama on new medication she’d been prescribed.
Oh, how I digress, but you get the point, which is that aside from twice-yearly routine visits to her primary care doctor, my mom generally refuses medical intervention. However, her back pain—which had been so bad for the previous month that she’d spent most of our twice-weekly visits lying supine on her sofa (and Christmas Day lying supine on ours)—had reached a point where she was ASKING to go to the ER. So needless to say, I was shook.
Of course I offered to come get her right then and there, but she insisted that she didn’t want to go until morning—and not FIRST thing in the morning, either, but rather, sometime around, say, 10.
I arrived to pick her up at 10 a.m. sharp the next morning and, because the hospital closest to us doesn’t have the BEST reputation, I took her to the hospital where I had gotten most of my cancer treatments, figuring ain’t no party like a Level 1 trauma center to set an old lady right.
As it turned out, everyone else, young and old, had the same idea; the hospital was so full that the old lady ended up sitting (well, LYING) IN A HALLWAY for a day and a half, while they pumped her full of pain killers and occasionally wheeled her away for various tests and scans. The good news was that her bed was at least close to the unit’s restroom, so she didn’t have far to shuffle when she had to go. In addition, we made great friends with the guy occupying the gurney on the other side of the hall (who’d come in the day before we had, because his blood pressure was through the roof), and his girlfriend (who worked at the hospital and stopped in periodically to check on him). Nice people.
Aside from that, though, it pretty much sucked. I slept in a chair at the foot of her bed (although she tried to convince me first to go home and sleep, and then to share the bed with her), and procured a toothbrush and toothpaste from our nurse the next morning, in order to avoid singeing my oncologist’s eyebrows off with my breath at that day’s previously-scheduled check-up appointment (which was right across the street, so I guess there was ONE advantage of choosing the hospital I did).
As it turned out, that wouldn’t be the only time that day I’d see him. Later that afternoon, after I’d returned to the foot of my mom’s hallway bed, I saw him walking down the ER corridor in our direction. “Oh, hey,” I thought. “There’s Dr. Cool-and-Calm.”
And then he coolly, calmly, stopped at my mom’s bed and said, “They sent me to see Nadine.”
Everything in me went cold.
I listened numbly as he told us that the scan results had come back, and shown a mass in her rectum, along with multiple lesions in her bones. She refused a biopsy, however, because she didn’t want any sort of treatment.
Within a couple of hours, the ER started to clear out a bit, and my mom scored an individual ER bay, with a door that shut and everything — which was a great relief to me, because after the news we’d gotten, I had started to feel like everything was too bright, too open, too raw, too exposed, TOO MUCH. I was looking forward to huddling up in a dark, quiet room with the door shut for a little while.
My mother, however, had other plans: despite multiple attempts made (by me and a couple of different nurses) to dim the lights, she wanted all the lights on full blast and the door left open. So that’s how we lived for just a couple more hours before she was finally moved into an actual hospital room, with a recliner for guests, a private bathroom and a window to the outside.
It felt like a five-star resort.
There we stayed for another night and most of the next day, while the doctors coordinated a care plan. Since she didn’t want any sort of treatment — she told anyone who asked, and a couple of people who didn’t, that she just wanted “to be kept comfortable” — she was fitted for a back brace (which we never actually ended up receiving), hooked up with a walker, prescribed pain meds (which was an ordeal; she staunchly refused multiple painkillers, insisting that she didn’t want anything habit-forming, but PFFFFFFed and rolled her eyes whenever anyone suggested Tylenol, complaining that it didn’t work for her . . . finally, she agreed to try Tramadol, not realizing it was an opioid (that nurse was pretty clever in how she presented it), and she said it worked well, so do you think I was about to open my trap and tell her the truth?), and sent home on Wednesday evening.
Home, sweet home
After getting her fed and tucked into her own bed at last, I went home myself for the first time in two days, to shower and sleep in preparation for meeting the home hospice nurse at my mom’s apartment on Thursday. She was lovely; she gave us a run-through of how everything would work, set up weekly visits (my mom was cranky about that, because she didn’t feel like she needed a weekly cadence just yet, but the nurse said that was the minimum), and went on her way with a promise to be in touch soon.
In the meantime, my oncologist friend, Dr. Awesome Pants (whom I’ve known since middle school), had texted to check on MY health and, when she found out everything that was going on with my mom, offered to be my mom’s doctor (see? AWESOME PANTS). So we scrambled to get her set up with Dr. Pants as a patient, and then set up a telehealth appointment (because Dr. Pants is in a different city) for Friday morning.
Friday morning, I showed up at my mom’s apartment bright and early, fresh from a glorious night’s sleep in my own bed, and cheerfully wielding breakfast from Starbucks (bacon-gruyere egg bites and cinnamon dolce lattes for all!). Once my mom had eaten some breakfast, she decided that since she had time, she wanted to take a shower before the appointment with Dr. Pants. She insisted that she didn’t need me to help her, or even to sit in the bathroom — she just wanted someone there “in case.” So I sat in the living room (only steps away from the bathroom; it’s a small apartment), and she left the bathroom door open so I could listen for trouble.
As she shuffled from her bedroom to her bathroom using only her cane, I chided her: “WHY aren’t you using your WALKER?”
“I don’t like the walker,” she grumbled. “It gets in the way.”
“Do I need to take your cane away?” I threatened.
Then she got mad.
“NO!” she snapped. “You are NOT going to take my cane away — it helps me BETTER than the walker.”
As she disappeared into the bathroom, I called out, “OK, but if you fall, THE CANE GOES.”
Well. Guess what happened?
Oh, it didn’t happen in that instant. She made it through the shower just fine, if a bit noisily (I heard the hollow thumps of what I’m assuming were elbows against the sides of the fiberglass shower insert, the wet squeeeeeege of maybe a shoulder or butt cheek sliding against shower wall, and a couple of verbal grunts, signaling what I figured was some breakthrough back pain). When I finally heard the curt croik! of the shower valve as she turned off the water, I opened my mouth to say, “You take the loudest showers I’ve ever heard!” when suddenly there was a loud CLANG followed by a huge THUMP.
I jumped up and darted to the bathroom, where I found her on the floor, curled up on her side.
Upon stepping out of the shower, she’d grabbed the bar of her towel rack to steady herself — something she apparently did EVERY time she took a shower — and it had given way.
Based on the odd, bony protrusion on the side of her that I could see, I should have realized she’d broken her hip — but I’d never before seen my mother lying naked on a bathroom floor, so I didn’t have a baseline for that scenario. I tried briefly to help her up, but even the slightest movement caused her so much pain that I gave up and, per instructions from our hospice visit day before, called the hospice nurse (the idea there is that if the goal is for the patient to remain at home, calling 911 is not going to be conducive, because it’s going result in a hospital). She offered two options: she could arrange for hospice workers to come and get my mom back into her bed and make her comfortable (i.e., drug her up) — which would hasten the inevitable, because at that point we knew she’d broken SOMETHING (we thought it was her leg), and leaving it untreated would result in rapid decline — OR we could call 911 and get her to the hospital.
She recommended the latter, saying that the first option was more for people who were REALLLLLLLY close to the end, and she didn’t think my mom was there yet.
So I hung up with the hospice nurse, carefully popped a nightgown over my mom’s head, and called 911; the paramedics arrived and, because my mom’s apartment is so small, they were unable to get the gurney even close to the bathroom, so they positioned it at the end of the hallway and, after loading her up with pain killers to make movement bearable, rolled her onto a blanket and pulled her, sled-style, down the hallway to hoist her onto the gurney.
The paramedic asked me which hospital I preferred. I gave him a brief (inasmuch as I’m capable of brevity) history of our past few days and said I DID NOT want her to wind up spending another two days in an ER hallway, and he said I could likely avoid that by taking her to the ER I’d eschewed (in favor of the “better” hospital) the first time around.
And I thought, what the heck? If all they needed to do was set her leg (which, again, was what we thought was broken) in a cast, that hospital would probably work as well as any other. So we took a short trek to the closest hospital this time . . .
The beginning of the end
And from there, it ALL kinda went to hell.
Nothing to do with the hospital itself; I have no complaints about the care she received there, and it turned out to be the best decision I could have made (more on that later); but once we got there, I would not spend a full day in my own home for nearly a month — and my sweet mama would never return to her little apartment again.
To speed this up a little, let’s itemize:
Day 1 (Friday): Here we go again. We arrived at the ER, where my mom was immediately given a room (HOORAY) and some X-rays. The ER doctor confirmed that the hip was broken; however, given the cancer diagnosis (and location), he wasn’t sure whether or not they’d be able to repair the hip.
So we settled in to wait for an answer to that question, while we listened to another patient down the hall yelling, “GO AWAY! I don’t KNOW the Godfather! It is NOT OK!” (From what I could tell, there was police involvement there, but I’m not quite sure what was going on; only that there was a lot of yelling about “The Godfather” and about tearing down the Wailing Wall.)
Eventually, she was moved to a hospital room, where she was visited by an orthopedic surgeon, who informed her that surgery WAS possible, and recommended she go through with it so she’d be able to move without pain (up to that point, it had been too painful to even raise the head of her bed, so she’d been lying flat on her back for hours). Miraculously, she agreed (she’d previously said that even if surgery DID turn out to be an option, she wasn’t doing it), and it was scheduled for the following day.
Day 2 (Saturday): Surgery day. The miracles continued: despite having a strict DNR in place, my mom agreed to suspend it during surgery (so that if something happened while she was on the table, life-saving measures could be taken).
As it turns out, though, the surgery went well; it was quick (about 40 minutes), and I spent most of it in the waiting room, talking to two lovely women who’d driven up from Texas (one because her father had fallen and broken HIS hip, and was having surgery—and the other for moral support). They’d brought TONS of snacks (so immediately, I knew they were my people), which they generously offered to share (I politely declined; y’all know I had my OWN snacks), and during our chat, I learned from one of them that the surgeon who was operating on both my mother and her father — the one who’d convinced my mom to have the surgery — was the sports medicine director for my kids’ school district (I later learned from my wrestling kid that he’s a wiz at stopping nosebleeds during meets)! But I digress. Point is, the surgery was fast and easy, and my mom was moved back to her room within no time, so I joined her up there and watched her snooze until my own bedtime, when I tiptoed out to go home and sleep.
Day 3 (Sunday): Things going downhill. I got a call from a nurse at 1:40 a.m., saying that my mom had been moved to the cardiac unit of the hospital, because they couldn’t get her heart rate down. I should have headed back to the hospital immediately, but I waited until about 8 to show up . . . at which point all hell had broken loose.
When I arrived, she was awake and PISSED TF OFF . . . and was not making a helluva lotta sense.
She was yelling at the nurse and threatening to sue the hospital, insisting that there had been a fire in the next room, but nobody had called the Fire Department; instead, they’d cleaned up the room to hide the evidence (which she’d somehow seen them do, even though the fire had been next door; in addition, she kept pointing at the painting on the wall—some generic, “soothing” framed hospital art—as more evidence of the fire). Further, she said that the nurse had confessed to her that he’d set the fire, and that he’d said something to her about how “those white people up on the hill think they know everything.” (It should be mentioned at this point that the nurse himself was a white people.)
Y’all. WTF.
My mother, despite her ripe old age (93) had NEV-UR had ANY cognitive issues before this moment; Sister was sharp as a tack, and had better memory and executive functioning than MY (middle-aged) ass. The nurse in question kind of shrugged at me, like, “Old ladies, amirite?” But I explained that she had previously shown ZERO signs of cognitive decline, and asked what else could be causing the current shit show (his theory: effects of the general anesthesia from the surgery). Eventually, she calmed down (the rest of the day passed with occasional reprises of confusing conversation, but far less agitation) — which was good, because her mental confusion soon took second fiddle to a new issue: low hemoglobin. So the bag of heart medication dangling from her IV pole was joined by two new blood bag buddies.
Days 4-5 (Monday-Tuesday): The hits kept coming, in the form of an elevated white count (the culprit: a UTI), elevated blood calcium levels (which I didn’t even know was a thing), and horrible constipation. So more treatments were piled on: antibiotics for the UTI, pills for the blood calcium, and an aggressive laxative regimen (with threats of a suppository) for the constipation. In addition, the Physical and Occupational therapists came to try to get her sitting up and moving, which increased her pain, so the whole “Don’t give me narcotics, but take your Tylenol and shove it” dance began anew.
The one bit of comic relief in that whole scenario was that while she was in the cardiac unit, she had the LOUDEST and most hilarious roommate!
Her name was Donna, and she was in a boat similar to Nadine’s; she’d come to the hospital for a reason I forget now, but had suddenly begun having chest tightness. She’d thought it was a heart attack, but scans showed a malignant mass on her lungs. Like Nadine, she was eschewing treatment, and like Nadine, she was pretty calm about it. LOUD. But calm. She eventually left the hospital for a nursing home, where she’d live out the rest of her life, however long it may be — but she was hoping to make it to her birthday in April.
All of this I know because once all her visitors had left for the day (between her children and grandchildren, she had a party going on most of the time), she’d take the opportunity to start calling people on the phone to keep them (LOUDLY) updated on her situation.
I also know that on the day she left the hospital for the nursing home, she took a banner poop, because when the nurse came in and asked when her last BM had been, she practically YELLED: “They didn’t tell you? I just shat Uranus! They had to cut it up with a knife to get it to flush!”
Y’all know that right there made me love her even more.
But what really bonded us was her obsession with the song 50 Ways to Leave Your Lover. The first evening we spent in that room, I sat eavesdropping (hardly a challenge, given Donna’s normal decibel level) on a conversation she was having with her daughter and son-in-law, while my mom dozed. I can’t recall how it came up, but she asked them if they remembered the song. As she (LOUDLY) tried to recall who’d sung the song (she thought it was Paul McCartney), I peeped around the curtain separating her bed from my mom’s, and answered: “It was Paul Simon, with back-up vocals by Phoebe Snow, Patti Austin, and Valerie Simpson.” (The song itself I can take or leave, but that back-up roster is an all-star line-up of my GURRRRRRRLZ.)
Eventually, she looked up the lyrics on her phone, and read them aloud to her family, while I sang along in my head. And from that point on, she mentioned the song to every new visitor who came to see her. And bless her heart, she always gave me credit for helping her remember who sang it (though she seemed wholly unimpressed with the back-up roster knowledge I’d dropped; she didn’t mention them ONCE).
But as usual, I digress. The point is, the days in the cardiac unit were chock full of new discoveries about things going wrong in my mother’s body, and attempts to balance “keeping her comfortable” with remedying what we could. And, of course, chock full of Donna’s musical proclivities and bowel shenanigans.
Day 6-7 (Wednesday-Thursday): Movin’ on up (or down, as the case may be). At long last, Nadine’s heart rate issues were under control, and she was moved back down to the unit where she’d originally been sent immediately following her surgery. While she was still being treated for the blood calcium, the constipation, and the UTI, she’d at least cut out the IV meds she was getting for the heart issues. From there, then, it was a matter of seeing what could be done from a physical and occupational therapy perspective in order to determine next steps (i.e., whether she’d do a stint in rehab and then return home, or end up following Donna to a skilled nursing facility).
Unfortunately, that whole endeavor turned out to be kind of a bust: without sufficient pain meds, she’d refuse to cooperate (because PAIN); but WITH sufficient pain meds, she’d be unable to cooperate (because she’d be asleep).
In addition, around this time, she developed a Kennedy ulcer — which again, I didn’t know was a thing, but it was a sure sign that things weren’t looking good. So in the end, the recommendation was to get her into a skilled nursing facility following her hospital stay.
Days 8-9 (Friday and Saturday): The search begins. Once we had a go-forward plan, we were visited by a kind hospital social worker, who provided a list of area nursing homes. My job was to look it over, do a little research (I was told that if I was interested in touring any of them, I should drop by unexpectedly instead of making an appointment, to get a clearer sense of how the place really operates), and come back with a list of top choices, at which point he would do some checking to see which of my choices had available beds. By the time I’d picked up my younger dude from school on the afternoon of Day 8 (Friday), I had already received a call from one of the nursing homes on the list. I was told that they did have availability, that they were ready to receive my mom immediately, and that a full month’s payment was required up front, at a rate of $325 per day for a shared room (she told me the only way for my mom to have a private room would be to “buy out” the other bed by paying double the cost).
As I had done NO research on ANY facilities at that point, I asked how long I could have to give it some thought, and she said taking the weekend would be fine.
I’d normally have spent Day 9 on a whirlwind nursing home tour, but I was utterly exhausted (physically, mentally, and emotionally) by the whole scene. So instead, after a quick visit to the hospital (during which I was able to call the social work team and ask if any of the facilities on the list offered private rooms (because if y’all think I’M a misanthrope, you didn’t know Nadine; she was the antisocial mother dough, whereas I am but a standoffish loaf) — and I was told NO), I joined my family on a day trip to the John Brown museum in Osawatomie, KS (with a stop in Fort Scott for books and ice cream on the way home) to celebrate Love Tank’s birthday.
It was a lovely respite.
Day 10: I believe in miracles. I showed back up at the hospital bright and early on Sunday, with the idea that I’d hang out with my mom for a bit, do a little online nursing home research from her room, and then spend a few hours popping around town for some surprise facility visits before returning to the hospital to work out a final decision.
Shortly after I arrived that morning, though, another social worker came to visit — a different one from the one who’d provided the original list of nursing homes, because apparently, that guy had the day off. She was up to speed on our case, and had a NEW list — narrowed down to the facilities that currently had open beds — to share with me. I thanked her (this was going to make my research much easier!), we chatted a bit, and she confirmed that most, if not all, of the places on the list would require my mom to have a roommate, agreeing that it wasn’t a desirable situation, especially at the cost per day (all of the places had comparable rates).
But then.
Then, she said there was ONE other option, but it might be kind of a long shot . . .
Seems there was a hospice house affiliated with the hospital, and located on the hospital campus. It only had eight beds, and tended to stay pretty full, and she wasn’t sure if my mom would qualify for admission (since it was a hospice facility, she’d have to meet more intense criteria), BUT:
- It had private rooms, and
- It would be covered by Medicare, and therefore would cost us nothing out of pocket.
I figured that even with all the caveats, it was worth a try! (My mom was hesitant, because she was under the impression that hospice facilities deny their patients any food, and she didn’t want to starve to death — but the social worker assured her that was NOT the case, and that she’d be able to eat whenever she wanted.) So the kind social worker stepped away to call the facility and see if she could get someone to come and do an assessment on my mom. She returned a few minutes later and said she’d reached the nurse practitioner who ran the place — who was still at home, but who would stop by my mom’s room on her way into work and visit with us.
YOU. GUYS.
I am here to tell you that by 3:00 that afternoon, my mom was settled into the hospice facility, and let me talk about it: she had a huge, lovely (and above all, PRIVATE) room equipped with a private bathroom, a fold-out couch for overnight guests, a recliner, an ottoman, a TV, and a small table with two chairs. In addition, there was a full kitchen and dining area outside her room, along with a living room area, complete with fireplace.
ALL. FOR. FREE. (And only about 7 minutes from my house.)
I was stunned silent (and more than a little verklempt), not only by the sheer loveliness of the facility (and the people there), but by the way it all worked out! Once again, I’d been given a chance to glimpse the Universe’s long game:
Had we not had the horrible experience of spending a day and a half in an ER hallway at an overcrowded hospital (or had that hospital not been overcrowded as, we were told, a result of icy weather causing people to get injured in multiple ways), I wouldn’t have chosen the hospital I did for the subsequent ER visit, which means I’d never have learned about this hospice facility.
Had I actually undertaken my nursing home research in a more timely manner, I’d likely have already chosen a place (I like to get difficult decisions made as quickly as possible) and started the ball rolling by the time the second social worker showed up, which means I’d never have learned about this hospice facility.
Had the timing of this whole ordeal been off by even one day, we may have never even encountered that second social worker, which means I’d never have learned about this hospice facility (because the first guy sure didn’t tell me). Not to mention the fact that the room my mom ended up in may have been occupied, and she wouldn’t have gotten in.
Of course it would have been ideal to stick with Plan A, where my mom could have spent her last days in her own apartment with in-home hospice care. But if that plan had to go down the crapper, this was the best possible Plan B I can imagine.
And here, my friends, is where I’m going to stop for now. Typically, I’m not a fan of two-part episodes, but this one is already WAY too long, and we haven’t even gotten through January; we’ve got a LONG way to go!
So in order to make this story a little more digestible, I’ll pause on the cookin’ for now, and be back later in the week with Part (2)2.
Waiting for next installment even though I know the ending. Thanks. Nadine taught me so much.